Medicine is both a science and an art. While evidence-based practice provides doctors with guidelines rooted in rigorous studies, empathy ensures that patients feel seen, heard, and cared for. Balancing these two dimensions is often the hardest — and most rewarding — part of being a physician.

The Rise of Evidence-Based Medicine
Evidence-based medicine (EBM) emerged to improve consistency in care by relying on high-quality research, clinical trials, and meta-analyses. Rather than decisions being guided solely by tradition or individual physician opinion, EBM provides a framework that emphasizes outcomes and safety.
For instance, guidelines on managing hypertension are derived from decades of randomized controlled trials. Similarly, antibiotic stewardship programs are built on evidence showing how misuse accelerates resistance.
Where Empathy Fits In
But patients are not statistics. They bring individual fears, cultural backgrounds, and unique life circumstances to every clinical encounter. A doctor prescribing the most scientifically validated treatment may still fail if the patient doesn’t feel understood or if the regimen doesn’t fit their lifestyle.
Empathy translates complex science into human care. It acknowledges the patient who can’t afford a brand-name drug, the single mother who can’t prioritize her own physical therapy, or the elderly man who fears losing independence more than facing side effects.
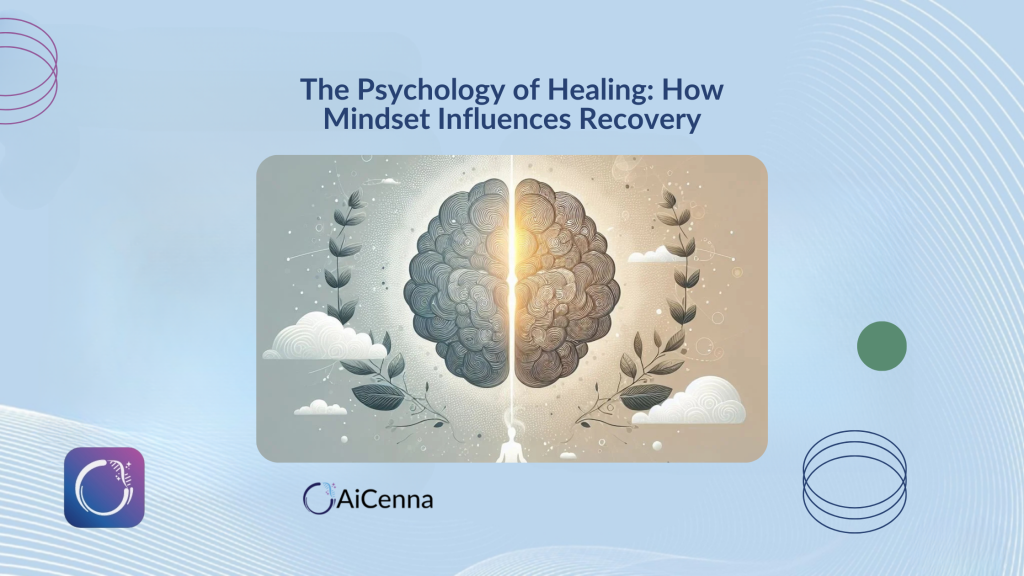
When Evidence and Empathy Clash
Sometimes evidence and empathy appear to diverge. Consider cancer treatment: clinical data may suggest aggressive chemotherapy as the best chance for survival, but a patient may value quality of life over a few more months. Here, empathy ensures the doctor respects patient autonomy.
The Doctor’s Role as Interpreter
Doctors are ultimately interpreters of science. They read journals, analyze trial outcomes, and evaluate guidelines — then translate them into language that patients can relate to. Empathy bridges the gap between data and lived experience.
Training for Both Skills
Medical education increasingly emphasizes communication skills and shared decision-making alongside scientific rigor. Empathy is no longer seen as “soft” medicine, but as a measurable contributor to adherence, recovery, and satisfaction.
Modern health technology platforms like AiCenna help strengthen this bridge, giving doctors real-time insights that make conversations more personalized without losing sight of the evidence.
Conclusion
Balancing empathy and evidence is not an either/or equation. It is about blending data-driven recommendations with the human touch, ensuring care is both effective and compassionate.